Endoscopic Surgery
1. Platelet Gel for Endoscopic Sinus Surgery
TheAnnals of Otology, Rhinology, and Laryngology. 2005 Sep;114(9):699-704
OBJECTIVES: New techniques are being utilized to improve outcomes for endoscopic sinus surgery, including newer forms of packing. Platelet gel is an innovative technique that holds many advantages, including comfort, hemostasis, and growth factors that may improve wound healing. This report discusses the theoretical advantages of this packing material and describes the initial results in a cohort of patients who underwent endoscopic sinus surgery.
METHODS: A cohort of patients who underwent endoscopic sinus surgery were interviewed and evaluated after the placement of platelet gel. A quality of life study was also administered for further understanding.
RESULTS: None of the patients in the study had postoperative epistaxis that required additional packing, and there were no instances of synechia formation or exuberant granulation tissue. Although not statistically significant because of a small population, the quality of life scores did show improvement over the control group.
CONCLUSIONS: Platelet gel used as a packing material after endoscopic sinus surgery offers efficient hemostatic properties, as well as growth factors that can advance the healing process. The quality of life of the patient may be improved by the use of platelet gel packing.
2. The Use of Autologous Platelet-Gel as an Intranasal Dressing in Functional Endoscopic Sinus Surgery
Presented at the American Rhinologic Society Meeting, September 2001, Denver, Colorado
Marc M. Kerner, MD, Northridge, CA
OBJECTIVE: The purpose of this initial prospective study is to assess the efficacy of autologous platelet gel as a postoperative dressing in patients undergoing functional endoscopic sinus surgery for chronic sinusitis.
DESIGN: The study consisted of a prospective, nonrandomized study in which patients were used as their own controls with platelet poor plasma.
Setting: A community referral otolaryngology practice of patients undergoing medical and surgical therapy for sinusitis.
Patients: Twenty-five consecutive patients undergoing endoscopic sinus surgery were enrolled in the study.
Intervention: The use of autologous platelet gel was delivered into the sinus cavities post-operatively.
Main Outcome Measures: Patients were examined weekly in the postoperative period for eight weeks, then at three months. Postoperative bleeding, time to onset of re-mucosalization, postoperative pain measurements, and synechiae formation were used as the main outcomes measures.
RESULTS: There were no platelet gel-induced synechiae in any of the treated patients, and time to onset of re-mucosalization appears to be reduced by almost one-third compared to historical controls. Additionally, there were no cases of postoperative bleeding, and patient discomfort measurements were reduced.
CONCLUSIONS: It appears in this initial phase study, platelet gel is a useful adjunct to endoscopic sinus surgery, as it may reduce postoperative bleeding complications, and accelerate mucosalization without inducing synechiae formation.
3. Intranasal Sinus Surgery: Revision Frontal Sinus Surgery Using Autologous Platelet Concentrate Enriched with Growth Factors (APC+)
MARC M. KERNER, MD, FACS, Assistant Clinical Professor of Surgery, UCLA School of Medicine
INTRODUCTION: Endoscopic frontal sinusotomy is a standard approach for dealing with chronic frontal sinusitis. Autologous platelet concentrate enriched with growth factors (APC+) is derived from the patients own blood. APC+ has been shown to accelerate wound healing and enhance bone graft survival.1 Few human studies have described its usefulness in soft tissue healing. We have presented data on its effectiveness and safety as a postoperative packing material in endoscopic sinus surgery.2 APC+ has excellent hemostatic properties, provides an excellent biologic dressing, and may prevent further synechiae formation within the sinuses.
The following case report describes a revision surgery for chronic left frontal sinusitis which was treated with endonasal endoscopic frontal sinus surgery using APC+ to stimulate and accerate the wound healing process.
OBJECTIVE: A 60 year old female had undergone three prior surgical procedures for chronic sinusitis since 1987. She had persistent left frontal sinusitis due to recurrent stenosis of the left frontal nasal outflow tract. Prior to our evaluation, the patient was offered an open procedure including a frontal sinus obliteration and/or a transfacial frontoethmoidectomy. She elected to undergo another attempt at endonasal procedure.
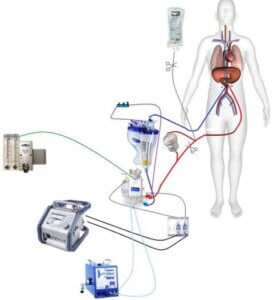
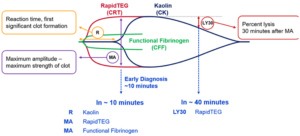
MATERIALS AND METHODS: Approximately 50cc of intravenous blood was drawn pre-operatively and processed using an automated dual spin process (SmartPReP®, Harvest Technologies, Inc., Plymouth, MA). The 12 minute process produced 10cc of autologous platelet concentrate enriched with growth factors (APC+) and approximately 20cc of platelet poor plasma (PPP).
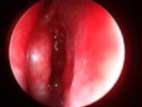
The patient underwent an endoscopic frontal sinusotomy using image guidance with the Instatrak system (VTI Systems, Boston, MA). Postoperatively, no packing was used except autologous platelet gel as a postoperative intrasinus dressing. An intraoperative view of APC+ in the middle meatus at the completion of surgery is shown in Figure 1.
 |
 |
 |
||
|
Figure 1 |
Figure 2 |
Figure 3 |
The patient was followed closely clinically in the postoperative period. Figure 2 shows the two week postoperative endoscopic view of surgical cavity in the region of the left frontal recess. The residual platelet clot is visible in the frontal recess region. Figure 3 shows the endoscopic view of left frontal recess at 6 months. The mucosa is well healed with no visual evidence of infection or restenosis. At the 6 month follow-up, the patient also showed no clinical symptoms of chronic sinus infections and complete resolution of her facial pain. Long-term follow-up at 2 years revealed persistent patency of the left frontal sinus outflow tract.
DISCUSSION: Endoscopic paranasal sinus surgery is the accepted modality for dealing with chronic sinusitis that has failed medical therapy. Our group has been using autologous platelet gel as an intranasal dressing for over two years and in over 175 similar procedures with excellent results.2 We have found it to be an excellent hemostatic agent, reduces postoperative swelling, and it does not appear to lead to increased synechiae formation. These are all ideal qualities for a postsurgical dressing in sinus surgery. Our practice
routinely uses APC+ to accelerate healing in otolaryngology procedures ranging from intronasal surgery to craniofacial surgery.
REFERENCES:
1. Marx RE, Carlson ER, Eichstaedt RM, et al: Platelet rich plasma: Growth factor enhancement for bone grafts. Oral Surg 85:638, 1998.
2. Kerner MM. The use of autologous platelet gel as a postoperative dressing in endoscopic sinus surgery. Presented at the American Rhinologic Society, September 9, 2001, Denver, CO