Anti-Microbial Effects of Platelet Gel
1. Antimicrobial Peptides from Human Platelets
Infection and Immunity, Dec. 2002, p. 6524–6533 Vol. 70, No. 12
Yi-Quan Tang, Michael R. Yeaman, and Michael E. Selsted
Platelets share structural and functional similarities with granulocytes known to participate in antimicrobial host defense. To evaluate the potential antimicrobial activities of platelet proteins, normal human platelets were stimulated with human thrombin in vitro. Components of the stimulated-platelet supernatants were purified to homogeneity by reversed-phase high-performance liquid chromatography. Purified peptides with inhibitory activity against Escherichia coli ML35 in an agar diffusion antimicrobial assay were characterized by mass spectrometry, amino acid analysis, and sequence determination. These analyses enabled the identification of seven thrombin-releasable antimicrobial peptides from human platelets: platelet factor 4 (PF-4), RANTES, connective tissue activating peptide 3 (CTAP-3), platelet basic protein, thymosin _-4 (T_-4), fibrinopeptide B (FP-B), and fibrinopeptide A (FP-A). With the exception of FP-A and FP-B, all peptides were also purified from acid extracts of nonstimulated platelets. The in vitro antimicrobial activities of the seven released peptides were further tested against bacteria (E. coli and Staphylococcus aureus) and fungi (Candida albicans and Cryptococcus neoformans). Each peptide exerted activity against at least two organisms. Generally, the peptides were more potent against bacteria than fungi, activity was greater at acidic pHs, and antimicrobial activities were dose dependent. Exceptions to these observations were observed with PF-4, which displayed a bimodal dose-response relationship in microbicidal assays, and T_-4, which had greater activity at alkaline pHs. At concentrations at which they were individually sublethal, PF-4 and CTAP-3 exerted synergistic microbicidal activity against E. coli. Collectively, these findings suggest a direct antimicrobial role for platelets as they are activated to release peptides in response to trauma or mediators of inflammation.
2. An In-Vitro Determination of Platelet Gel Efficacy as Prevention of Post-Operative Bacterial Infections
Jessica N. Isaly and Dr. Philip Beckley, Ph.D.
The Ohio State University
School of Allied Medicine, Circulation Technology Division
Background: Clinical studies have shown that platelet gel may have advantageous effects on wound healing due to the growth factors platelets release when activated. Since platelet gel also contains leukocytes, or white blood cells, it is hypothesized that application of the gel to surgical wounds will reduce or possibly eliminate bacterial growth. Pseudomonas, Staphylococcus Aureus, and Enterococci are three of the most common bacteria found in surgical wounds. The incidence of bacterial infection in cardiac surgery patients has been shown to be as high as 21.7%. This confirms a need for better prevention of such infections, especially since many strains of bacteria are becoming resistant to conventional antibiotic treatments.
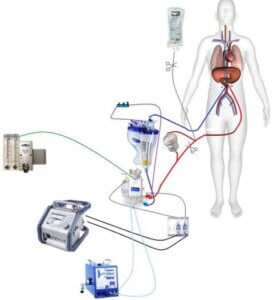
Methods: Fifty-five milliliters of human blood was collected into a syringe containing five milliliters of ACD. The blood was separated into red blood cells (RBC), platelet poor plasma (PPP), and platelet rich plasma (PRP). Platelet gel was then made by adding calcium and thrombin to the PRP. Four groups were established: the Control group, containing only the bacteria; Group A, containing PPP and the bacteria; Group B, containing PRP and the bacteria; and Group C, containing RBC and the bacteria. BacteriaPseudomonas, Staphylococcus Aureus, and Enterococci were plated using blood agar plates and incubated for three days at 37° Celsius.
Results: The PPP plates showed no visible inhibition of bacterial growth for any of the three bacteria. However, there was visible inhibition, with a marked bactericidal effect for two of the three bacteria in the PRP plates. Also, in the RBC plates, there was some visible inhibition of bacterial growth for two of the three bacteria.
Discussion: Platelet rich plasma appears to be effective in preventing growth of Pseudomonas and Staphylococcus Aureus. Bactericidal effects are also noted. Contamination and/or human error explains the lack of inhibition of Enterococci growth. Further studies need to be conducted to confirm this hypothesis.
This study can be considered pioneer in that very little research has been done on the antibacterial properties of platelets gels. Platelet gel as an “unconventional antibiotic” provides exciting and promising effects for all surgical and burn victims. This is especially important in cardiac surgery, where the occurrence of infection is significant. One study results that 21.7% of cardiac patients developed some type of nosocomial infection which required an increased length of stay in the hospital6. The applications of platelet gel usage will continue to increase over the coming years. This will necessitate cost-effective and practical protocols to be implemented in healthcare centers all over the world.
Conclusions: Platelet rich plasma is effective in preventing Pseudomonas and Staphylococcus Aureus bacterial growth. It also has a bactericidal effect, which makes it a valuable asset to wound maintenance and healing